High Resolution Esophageal Manometry
Disorders of pharyngeal and esophageal motor function is a common cause of symptoms, particularly dysphagia, non-cardiac chest pain, and those associated with gastroesophageal reflux.
Motor function can be assessed by a variety of recording techniques including radiology, scintigraphy manometry, and most recently intraluminal electrical impedance monitoring. Some of these are complementary. The gold standard, however, for the assessment of motor disorders remains manometry.
Manometric measurement of esophageal pressure is the most direct method for assessment of motor function. Only manometry can give information on the strength of contractions. But manometry also has its disadvantages. In assessing the consequences of motility, the movement of intraluminal content is only by inference. However, when the diagnosis requires information about intraluminal flow, this can be obtained by complementary measurement of transit by radiology, scintigraphy, or intraluminal impedance monitoring.
Esophageal Manometry
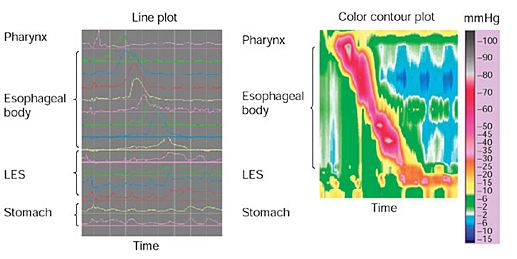
This high resolution system minimizes the time of the test from 45 minutes to 5 minutes in length which helps the patient recover faster. The revolutionary test allows 3D imagery to capture the procedure and is the first to allow the ability to assess pathology in the pharynx and upper esophageal sphincter as well to assess bolus clearance in cases which are resistant to PPI therapy.
Indications:
Esophageal manometry is indicated in patients whose symptoms and other investigations, for example, endoscopy or radiologic studies, suggest a motor disorder. It is not a primary investigation and should be performed only when the diagnosis has not been achieved by careful history, barium radiology, or endoscopy.
Dysphagia is the most rewarding indication for manometry. Dysphagia associated with motor disorders is typically intermittent, variable, and associated with both liquids and solids, although it is commonly worse with solids. There is a clear indication for manometry in patients with a normal endoscopy who have consistent dysphagia with solids if there is associated regurgitation or weight loss or if there is significant impairment of lifestyle. The likelihood of finding a major motor disorder such as achalasia or diffuse spasm, which may be amenable to treatment, is relatively high. However, not all dysphagia needs to be tested by manometry. Mild intermittent dysphagia due to weak esophageal contractions is relatively common, particularly in patients with gastroesophageal reflux disease. Investigating these patients is usually not indicated except in patients who are anxious to have this investigated as far as possible or perhaps in patients undergoing antireflux surgery.
Non-cardiac chest pain is a common reason for referral for manometric studies. However, the diagnostic yield is relatively low, particularly when dysphagia is absent. Achalasia and diffuse spasm account for less than 5% of patients. The clinical significance of other nonspecific patterns of abnormal esophageal motility is unclear.
Gastroesophageal reflux disease: Esophageal manometry has a limited application in patients with reflux disease. There are no diagnostic manometric features. Manometry is useful to define the location of the LES for the purposes of positioning a pH electrode for ambulatory pH monitoring. Manometry is also commonly performed before antireflux surgery to exclude other diagnoses such as achalasia, which may present with reflux-type symptoms, and to exclude major weaknesses in esophageal peristalsis, which may compromise the surgical outcome. Current evidence would suggest that routine preoperative manometry in patients with clearly defined reflux disease is not justified. However, it is reasonable to assess patients suspected of having severely compromised esophageal motor function, such as those with symptoms to suggest scleroderma or with a dilated or poorly motile esophagus on barium swallow.
> Go to: Esophageal Manometry
> Go to: Preparing For Your Esophageal Manometry Procedure/
> Go to: What is Non-Cardiac Chest Pain
