Missed Colorectal Cancers Usually Have Subtle Appearance
- admin
- January 28, 2015
- Cancer, Recent News
- No responses
By Caroline Helwick
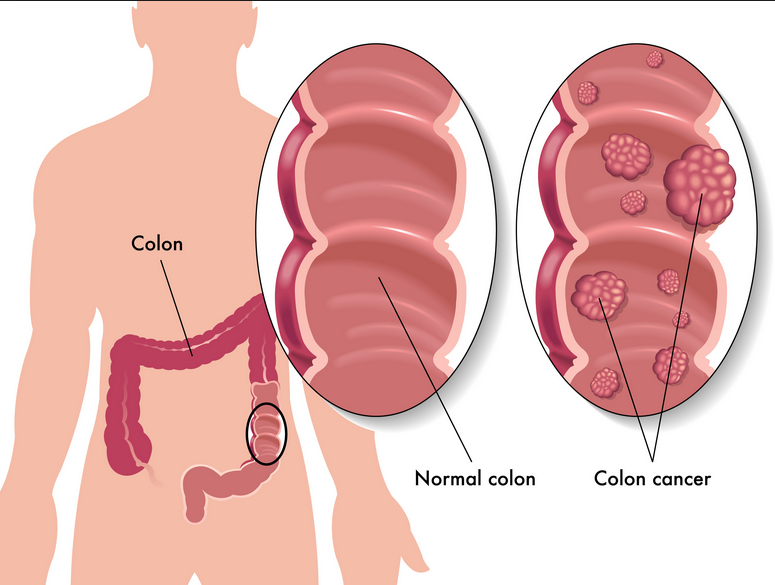
June 10, 2011 (Chicago, Illinois) — Reasons for the occurrence of interval colorectal cancers (CRCs) have been unclear, but a study from the Netherlands establishes that most such lesions have a subtle macroscopic appearance, in that they are primarily small and flat, and are easy to miss on follow-up colonoscopy.
The findings from a 10-year review of cases were presented in a “Best of DDW” session here at Digestive Disease Week (DDW) 2011 by Chantal le Clercq, a medical student at Maastricht University Medical Center in the Netherlands. The senior investigator was Silvia Sanduleanu, MD, PhD.
“We found that the majority of interval cancers could be related to lesions that were overlooked, probably because they were small or flat, and — to a lesser degree — incomplete polypectomy,” she said. “This means that systematic training on detection and effective treatment is essential [for] preventing these interval CRCs in everyday practice.”
Douglas Rex, MD, distinguished professor of medicine at Indiana University School of Medicine, Indianapolis, and a past president of the American Gastroenterological Association, echoed these remarks in an invited lecture on colonoscopy. He called colonoscopy “the most important procedure we teach in fellowship. Let’s embrace colonoscopy and perfect it,” he said.
Interval Cancers Common
In this study, interval CRCs were defined as those detected between 6 months and 5 years after an index colonoscopy. Their incidence in other studies has been reported to range from around 5% to as high as 8% among all CRCs. “Interval cancers appear to be more common than we previously expected,” she said. “Factors thought to be associated with them are operator-dependent variability and ineffectiveness of treatment, but the precise reasons are unclear.”
To gain insight into this issue, the investigators reviewed data from all patients diagnosed with CRC at Maastricht University Medical Center between 2001 and 2010, excluding those with hereditary CRC, inflammatory bowel disease, and previous history of CRC. The researchers evaluated the macroscopic appearance — specifically, flat vs protruded — and location of the cancers in the colon, and they compared these characteristics with those of the previously diagnosed (noninterval) CRCs.
The interval CRCs were classified as being missed lesions (having a subtle appearance) either because of incomplete polypectomy (when the lesion occurred in the same segment as the previous polypectomy) or of unknown cause.
Of 1218 patients diagnosed with CRC, 39 (3.1%) had undergone colonoscopy within 5 years. Eleven of these patients were excluded because of incomplete visualization or inadequate surveillance, leaving 28 patients and yielding an interval CRC rate of 2.2%. Patients’ mean age was 73 years, 71% were men, and their mean time from colonoscopy was 26 months. Most of the patients presented for colonoscopy because they had symptoms.
Why Lesions May Have Been Missed
“The size of the interval CRCs, compared with the noninterval index cancers, was considerably smaller, and the lesions were more likely to be flat,” Ms. le Clercq reported.
Lesions smaller than 1 cm were noted in 11.6% of interval CRCs vs 1.3% of noninterval cancers, and lesions 1 to 2 cm in size were seen in 19.2% vs 12.5%, respectively. Cancers larger than 2 cm occurred in 69.2% vs 86.2%, respectively (P < .001). The mean size of the interval lesions was 2.7 cm vs 3.9 cm for the noninterval lesions. The appearance was flat in 48.1% of the interval CRCs vs 20.9% of the noninterval cancers, and protruded in 51.9% vs 79.1%, respectively (P < .001). Other characteristics were similar, including stage (early vs advanced), histology (poor vs well-differentiated), and specialty of provider (approximately 75% were gastroenterologists). By location, the lesions were found in the proximal colon in 70.4% of the interval cases vs 32.9% of the noninterval cases (P < .001). In a regression analysis, adjusted for age and sex, the odds ratios were as follows: small lesion: odds ratio, 0.82 (P = .020), flat vs protruded appearance: odds ratio, 3.75 (P = .001), and proximal vs distal location: odds ratio, 5.07 (P < .001). "A subtle appearance explained 53.6% of the CRCs, and these could be classified as 'missed' lesions, while 10.7% were in the same segment, and therefore may have been incompletely removed. For 35.7%, we found no clear explanation," she concluded.
Could Missed Lesions Be More Aggressive?
Dr. Sanduleanu’s center is now focusing colonoscopy training on the detection of small and flat lesions. “We will be looking at the future interval cancer rate in this well-trained group,” she said. The investigators also plan to do molecular testing on interval lesions to assess whether these might represent inherently more aggressive, new cancers.
Dr. Rex, in his lecture, noted that some missed cancers may be fast-growing. These would include serrated lesions, many of which are associated with BRAF mutations and can have a subtle appearance, but can rapidly progress. “We may miss serrated lesions more than adenomas,” he suggested. Detection rates of serrated lesions have been reported to vary 7- to 18-fold among practitioners, he added.
“It is important for the endoscopist to develop an eye for these in order to detect and remove them effectively,” he said. Detection of depressed adenomas and providing greater protection to the right colon are also areas that need improvement.
Commenting on the Dutch findings, he noted that the group’s performance of colonoscopy seemed to be “quite good,” as their rate of interval CRCs was just 2.2%, which is lower than previous reports. Had they included cancers detected within 6 months of the colonoscopy, not after 6 months, as some groups do, the rate might have been higher, he suggested.
He also said the 11% rate of incomplete polypectomies may actually include some missed cancers. “You are getting the maximum rate of missed cancers, because it is possible another lesion was in the same segment, maybe the next fold over, and you missed it. You are just assuming the polyp was removed incompletely, but almost certainly some of those were missed lesions.”
Ms. le Clercq has disclosed no relevant financial relationships. Dr. Rex reported receiving consulting, speaking, and teaching fees for numerous pharmaceutical and device companies, and serving on several review boards.
